Biomed adv. 2(2):96-101.
doi: 10.34172/bma.18
Review Article
Thrombosed aneurysmal right coronary artery presenting as inferior STEMI: A comprehensive review and case report of diagnosis, imaging and management
Seyedeh-Tarlan Mirzohreh Data curation, Writing – original draft, Writing – review & editing, 1 
Ahmad Separham Conceptualization, Data curation, Investigation, Writing – review & editing, 2 
Zahra Hosnavi Methodology, 2
Elnaz Javanshir Conceptualization, Data curation, Investigation, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing, 2, * 
Author information:
1Student Research Committee, Faculty of Medicine, Tabriz University of Medical Sciences, Tabriz, Iran
2Cardiovascular Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
Abstract
Summary
Coronary artery aneurysms (CAAs) are rare vascular disorders characterized by localized dilatation of a coronary artery segment, often leading to severe complications such as thrombosis, embolization, and rupture. This case report discusses a thrombosed aneurysmal right coronary artery (RCA) presenting as an inferior STEMI. A 61-year-old male presented with chest pain and diaphoresis. An ECG revealed inferior STEMI, and emergent coronary angiography (CAG) identified a large RCA aneurysm (2.14 x 1.4 cm) with significant thrombus and distal occlusion. PCI was performed, including aspiration thrombectomy and balloon angioplasty, followed by dual antiplatelet therapy (DAPT) and anticoagulation. Echocardiography confirmed the aneurysm and showed mildly reduced ejection fraction. Follow-up CAG demonstrated thrombus resolution, and the patient remained asymptomatic over 1.5 years. Thrombosed RCA aneurysms are challenging to diagnose due to varied presentations mimicking acute coronary syndromes. Imaging modalities such as echocardiography, cardiac CT, and CAG are crucial for accurate diagnosis and management. Treatment strategies include surgical resection, percutaneous interventions, and medical therapy, tailored to the patient’s clinical and imaging findings.Thrombosed RCA aneurysms require prompt diagnosis and intervention. Advanced imaging and a tailored treatment approach are essential for optimal outcomes. This case highlights the importance of comprehensive management in patients with CAA-associated STEMI.
Keywords: Right Coronary artery aneurysm, ST-elevation myocardial infarction, Thrombosis
Copyright and License Information
© 2025 The Author(s).
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Funding Statement
The authors received no financial support for the research, authorship, and/or publication of this article.
Introduction
A coronary artery aneurysm (CAA) is a rare and potentially life-threatening vascular disorder characterized by a localized dilatation of a coronary artery segment, exceeding 1.5 times the diameter of the adjacent normal segment.1,2 This condition can be caused by various factors, including atherosclerosis, which is the most common cause, as well as congenital, mycotic, or systemic inflammatory diseases.2 It is reported that CAA can lead to severe clinical sequelae, including thrombus formation, embolization, fistula formation, and rupture.3 The pathophysiology of CAAs is still not fully understood, and giant aneurysms are particularly rare.4 CAAs can involve any of the coronary arteries; however, anomalies of the left main stem are quite rare, occurring in approximately 0.1% of the population.5 Rarely, the aneurysm can become completely occluded by a thrombus.3 Thromboembolism is a recognized complication in patients predisposed to CAA who experience ST-elevation myocardial infarction (STEMI). In cases where a thrombus blocks the aneurysm, blood flow can be greatly reduced, resulting in a TIMI-I flow, which is marked by a large thrombus that almost completely blocks the distal part of the vessel. Additionally, the reduced flow in an enlarged aneurysmal vessel encourages the formation of thrombus.6 Treatment options for CAAs include surgical correction, which is generally accepted as the preferred treatment,3 as well as thrombus aspiration and balloon dilation7; however, the management of patients presenting with STEMI secondary to CAA using primary coronary angioplasty can be challenging.8 It is essential to understand the pathophysiology, classification, clinical presentation, assessment, and management of CAAs to provide optimal care for patients with this condition.9
We describe the case of a 61-year-old individual with a right CAA and thrombus formation, who presented with an inferior STEMI. The patient initially underwent percutaneous coronary intervention (PCI) and was subsequently managed with intensification of anticoagulation therapy.
Case Presentation
A 61-year-old male with no prior medical history presented to the emergency department with a 24-hour history of left sternal chest pain radiating to his left arm, accompanied by diaphoresis. He denied any history of hypertension, diabetes mellitus, or tobacco use. On admission, his vital signs were stable, with a blood pressure of 130/80 mm Hg, heart rate of 88 beats per minute, and oxygen saturation of 98% on room air. Cardiac auscultation revealed no murmurs, rubs, or gallops. An ECG demonstrated ST-segment elevation in the inferior leads (II, III, and aVF), consistent with an acute inferior STEMI. Emergent coronary angiography (CAG) revealed a large aneurysm measuring 2.14 × 1.4 cm in the mid-distal segment of RCA, containing a significant thrombus. Distal to the aneurysm, a 100% occlusion was observed, likely due to embolization of thrombotic material from the aneurysm. Proximal left anterior descending artery (LAD) and left circumflex artery (LCX) were ecstatic. PCI was performed (Supplementary file 1, Video 1), starting with aspiration thrombectomy to remove the thrombus, followed by plain old balloon angioplasty (POBA) of the distal occlusion to restore coronary flow (Supplementary file 2, Video 2). Given the high thrombotic burden, eptifibatide, a glycoprotein IIb/IIIa inhibitor, was administered intracoronary during the procedure. Due to the extensive thrombus, deployment of a covered stent was deferred to mitigate the risk of further complications. The patient was admitted to the coronary care unit and started on dual antiplatelet therapy (DAPT) with aspirin and clopidogrel, along with enoxaparin 70 mg (BD) for anticoagulation. Intravenous infusion of eptifibatide was continued for 24 hours post-PCI. A departmental echocardiogram showed normal LV and RV size and mildly reduced ejection fraction (40%-45%) with akinetic base and mid-inferior wall segments. Moreover, echo free round shape structure in the right-side AV groove near to tricuspid annulus in favor of right CAA (15*14 mm) was seen on echocardiogram (Figure 1). A follow-up CAG conducted one week later demonstrated significant resolution of the thrombus within the aneurysm (Supplementary file 3, Video 3). The patient was subsequently discharged on a regimen of apixaban 5 mg (BD), and clopidogrel 75 mg (OD), to minimize the risk of recurrent thrombotic events. Throughout his hospitalization and subsequent 1.5-year follow-up, the patient remained asymptomatic, with no recurrence of chest pain or thrombotic complications.
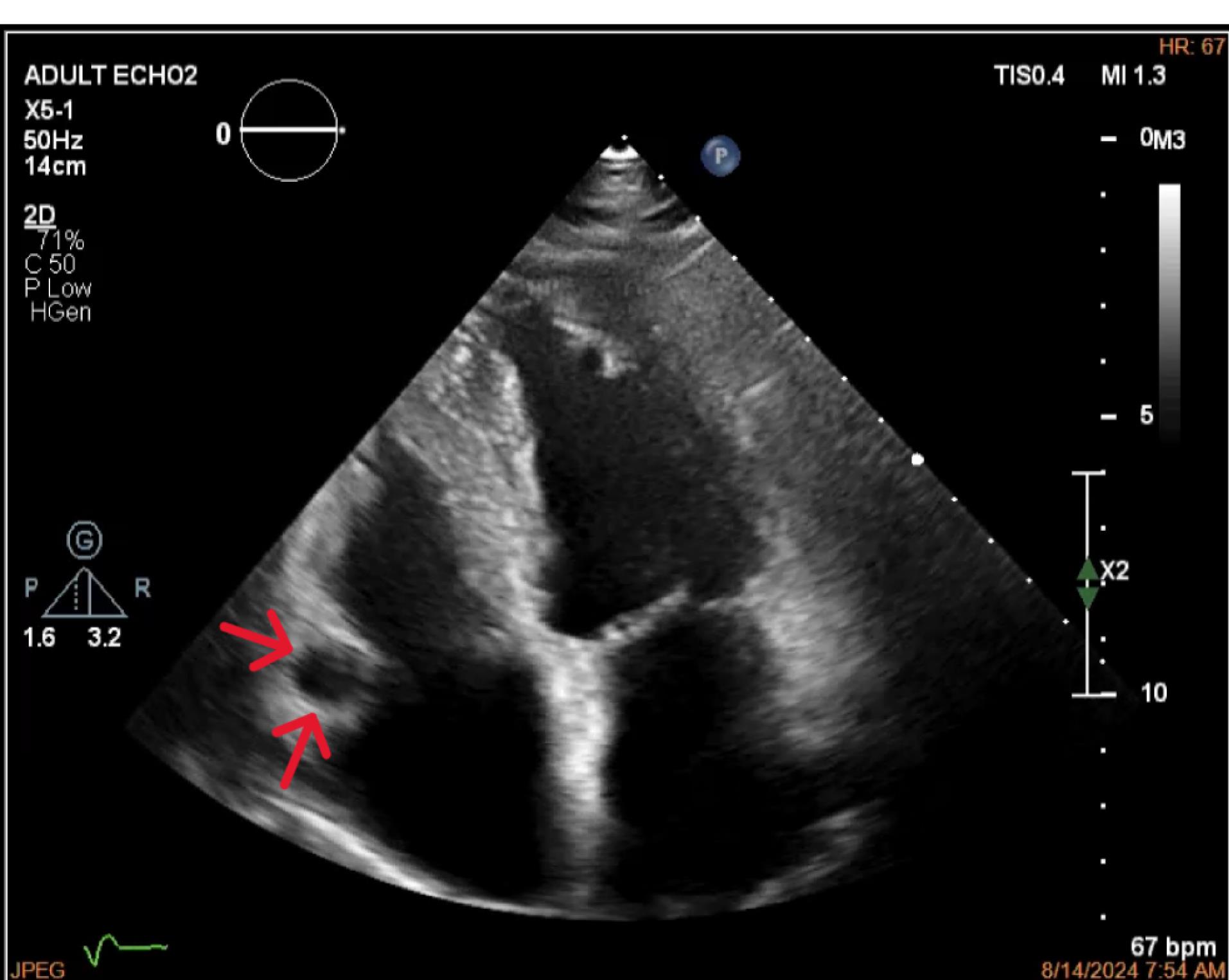
Figure 1.
Echocardiogram (four-chamber view) with red arrows indicating the location of the right coronary artery
.
Echocardiogram (four-chamber view) with red arrows indicating the location of the right coronary artery
Topic analysis
Table 1 presents a series of 9 cases involving thrombosed RCA aneurysms,10-18 often associated with acute coronary syndromes such as Inferior STEMI11-13,15 or NSTEMI.14 Patients ranged in age from 31 to 81 years, with both males and females represented. The clinical presentation varies from acute chest pain,12-15,18 dyspnea,18 limb edema,10,17 decreased exercise tolerance16 to hospital referral for imaging due to suspicious ECG findings or progressive symptoms suggestive of CAD.18
Table 1.
Case reports of thrombosed RCA aneurysm
|
First author, year
|
Patients
Gender and Age
|
Past Medical History
|
Presentation, initial diagnosis
|
Imaging for first Diagnosis of Aneurysm
|
Characteristics of Aneurysm (CAG)
|
Management and
Follow-Up
|
| Wang et al, 202410 |
Female,
56 years old |
Lower limbs
Edema |
Referred to hospital with
chest congestion and limb edema
●Heavy ball mass adjacent to the RV accompanied
(Echo-detected) |
Echocardiography on admission: a large circular occupying lesion, resembling a bulky hypoechoic ball originating from RCA casing compression on RV.
ECG-gated cardiac-CT and 3D reconstruction further confirmed the mass as a hypodense shadow. |
One aneurysm measuring
6.3 cm × 5.4 cm (proximal RCA) with thrombosis |
●Surgical resection and repair
●Post-operation: Not reported |
| Ishida et al, 202411 |
Male, 52 years old |
HTN, dyslipidemia |
Transient ischemic attack
●Anterior and Inferior STEMI |
CTA: A giant CAA at the RCA (50mm), completely occluded by a thrombus1. |
RCA was occluded at proximal to the CAA, and the CAA did not show contrast.
however, the artery distal to the CAA showed contrast via a collateral artery from the LCX. |
●At first, IV heparin started.
4 days later, CTA and CAG were performed again. They showed slight contrast in the CAA and the distal coronary artery. Then, CABG (right gastroepiploic artery–RCA distal to the CAA) and CAA was resected.
●Post-operation: Not reported |
| Steenbergen et al, 202412 |
Female, 81-year-old |
None |
Progressive, non-exertional
chest pain
●Inferior STEMI |
Emergent CAG:
Giant saccular aneurysm in the proximal RCA with significant thrombus
Cardiac CT:
Aneurysm was 5cm in size. |
Giant saccular aneurysm in proximal RCA with thrombosis |
●Conservative medical treatment.
Low-dose rivaroxaban was added to existing antiplatelet therapy.
(Attempts to enter into the RCA were unsuccessful)
●Post-operatopn: Not reported |
| Khan et al, 202413 |
Male, 31 years old |
None |
Sudden-onset chest pain
●Inferior STEMI |
Emergent CAG:
RCA ostial aneurysm of about 8 mm in size with heavy thrombus formation + an occluded distal PDA |
RCA ostial aneurysm of about 8 mm in size with heavy thrombus formation + an occluded distal PDA |
●Administration of two boluses
of a glycoprotein IIb/IIIa
inhibitor (tirofiban) during CAG, followed by a tirofiban infusion
(12.5 mg) for six hours.
+
●DAPT (aspirin + clopidogrel) + enoxaparin during hospitalization
●Discharged with clopidogrel 75 mg (OD) rivaroxaban 20 mg (OD). |
| Jalalzai et al, 202314 |
Male, 56 years old |
None |
Retrosternal chest and, left arm pain of sudden onset, chest tightness, and shortness of breath.
●NSTEMI |
CAG: two aneurysms measuring 52 × 45 mm and 22 × 20 mm |
Two aneurysms measuring 52 × 45 mm, 22 × 20 mm
(Middle and proximal segments) |
●CABG (Vein graft was used to bypass the distal RCA), thrombectomy.
●Post-operation: Not reported |
| Al Hennawi et al, 202215 |
Male,
40 years old |
Gout |
Acute onset of severe
chest pain, sweating, pain radiation to the left arm with a tingling sensation, and concurrent acute-onset diarrhea.
●STEMI |
CAG: Mid-RCA aneurysm, and mid-distal thrombotic occlusion of the RCA. |
Mid-RCA aneurysm, and mid-distal thrombotic occlusion of the RCA. |
●PCI: POBA on RCA.
Distal occlusion was stented with Resolute Onyx.
●No postoperative complication.
Discharged on DAPT
for one year. |
| Teng et al, 202016 |
Female,
53 years old |
None |
Decreased exercise tolerance and lower extremity edema for 3 months, elevated eosinophil cell number.
●Intra-RV mass suspicious for cardiac tumor. |
Surgical view2 and IHC study confirmed the diagnosis of CAA with CD34, CD31 positive and D2–40 negative. |
Intra-ventricular mass 3.5 × 2.5 cm in size locating at the right ventricle below the tricuspid annulus. |
●Aneurysm was surgically resected.
No CABG was performed.
●3 months later: A dilated RCA with the proximal diameter of 6.1 mm and a fistula between RCA and RV with a diameter of 2.3 mm was seen on TTE. |
| Tham et al, 201917 |
Male,
80 years old |
CABG, repaired abdominal artery aneurysm and repaired bilateral iliac arteries aneurysms |
None.
● Non-obstructive atrial mass proximal to the tricuspid valve at the right AV junction
(Echo-detected) |
CTA revealed a large calcified and thrombosed RCA aneurysm compressing the RA externally. |
Not reported |
●Aneurysmal mass was
surgically resected
+
CABG
(Femoral-popliteal bypass)
●Post-operation: Not reported |
| Arcinas et al, 201818 |
Female,
54 years old |
None |
Progressive dyspnea following an episode of severe chest pain
(For 3 weeks).
Previous inferior MI (ECG-revealed).
●Referred for CTA based on ECG findings, suspicious for CAD. |
TTE: A 7 x 5 cm circumscribed intrapericardial mass in the right AV groove.
Cardiac CT: Confirmed mass with peripheral calcification, external to AV groove.
CMRI: No gadolinium enhancement, suggestive of
thrombosis in the mass |
Giant dense mass
8 cm x 5 cm in the
right AV groove. |
●Aneurysmal mass was
surgically resected.
+
CABG
●Post-operation: Not reported |
1After posterior leaflet of tricuspid was detached from annulus, it was confirmed as a thrombosed right CAA.
2Normal views in echocardiography, CTA showed an irregular mass with internal contrast enhancement locating below the tricuspid annulus.
Initial diagnosis
The initial diagnosis of thrombosed RCA aneurysms is often challenging due to their varied clinical presentations, which can mimic acute coronary syndromes or other cardiac pathologies. Echocardiography is typically the first-line imaging modality, providing a non-invasive and rapid assessment of cardiac structures. In many cases, echocardiography reveals a large, hypoechoic mass adjacent to the RV10,16 or within the RCA,12,17 often accompanied by signs of RV compression. In the studies by Teng et al16 and Tham et al,17 the initial suspicions were an intra-RV cardiac tumor and a right atrial RA mass, respectively. This initial finding raises suspicion of a thrombosed aneurysm and prompts further investigation.
Imaging
Cardiac CT and CAG are then employed to confirm the diagnosis and provide detailed anatomical information. Cardiac CT, with its ability to generate three-dimensional reconstructions, offers precise measurements of the aneurysm’s size, location, and relationship to surrounding structures, while CAG allows for dynamic visualization of coronary blood flow, often revealing complete occlusion of the RCA with distal perfusion maintained via collaterals. In complex cases, MRI may be utilized to further characterize the aneurysm, particularly when thrombus formation or tissue composition needs to be assessed.18 The integration of these imaging modalities ensures an accurate and comprehensive diagnosis, guiding subsequent management decisions.
Management
Management strategies varied depending on the clinical scenario and imaging findings. Surgical resection of the aneurysm, often combined with CABG, was a common approach, particularly in cases with significant thrombus burden or compression of adjacent structures. Percutaneous interventions, including thrombectomy and stenting, were employed in select cases, while medical therapy with anticoagulants and antiplatelet agents was used either as adjunctive treatment or in cases where invasive procedures were not feasible.
Management algorithm for CAA with associated STEMI
Figure 2 represents the complex management of patients with STEMI related to a CAA.19
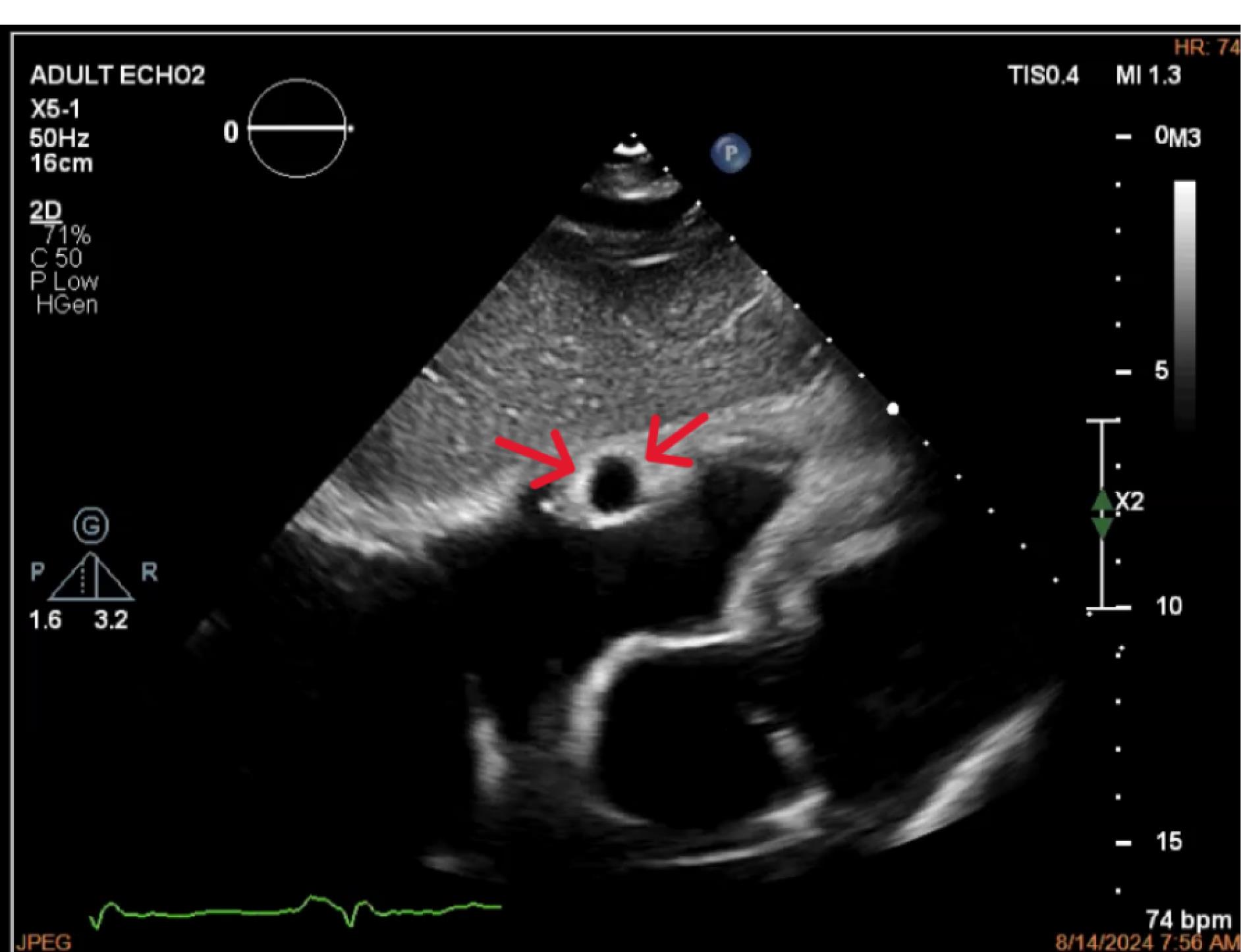
Figure 2.
Echocardiogram (subxiphoid view) with red arrows indicating the location of the right coronary artery
.
Echocardiogram (subxiphoid view) with red arrows indicating the location of the right coronary artery
The management of a CAA associated with STEMI focuses on relieving the thrombotic burden to achieve TIMI II-III anterograde flow. Initial interventions may include aspiration thrombectomy, balloon angioplasty, thrombectomy, or direct catheter aspiration, with consideration given to adjuvant intracoronary fibrinolytics or antiplatelet agents. A thorough etiologic workup, utilizing angiography and intravascular ultrasound (IVUS), is essential to evaluate the aneurysm and identify any associated conditions, such as coronary stenosis or ruptured plaque. In cases where stenosis or plaque rupture is present, treatment options include the use of a self-expanding stent for vessels < 5 mm or a drug-eluting stent (DES) for vessels ≥ 5 mm, accompanied by anticoagulant and antiplatelet therapy in line with PCI and atrial fibrillation guidelines. Additionally, addressing the underlying cause of the aneurysm is critical. In the absence of associated stenosis, management varies based on thrombus burden: low thrombus burden may be managed with standard therapy, while high thrombus burden may necessitate the use of IIb/IIIa inhibitors and heparin perfusion, with consideration of a staged procedure. A covered stent may be employed in the absence of significant tortuosity, calcification, or side branch involvement. This approach underscores the importance of a tailored strategy, guided by thrombus burden, vessel characteristics, and associated pathology, to optimize outcomes in patients with CAAs and STEMI.9 PCI of an aneurysmatic culprit vessel has been shown to have a limited success rate, accompanied by a significantly high incidence of stent thrombosis (> 15%) at the 1-year follow-up mark.19 Consequently, the preferred revascularization strategy should prioritize the restoration of anterograde flow, with stent implantation being considered a secondary consideration (Figure 3).
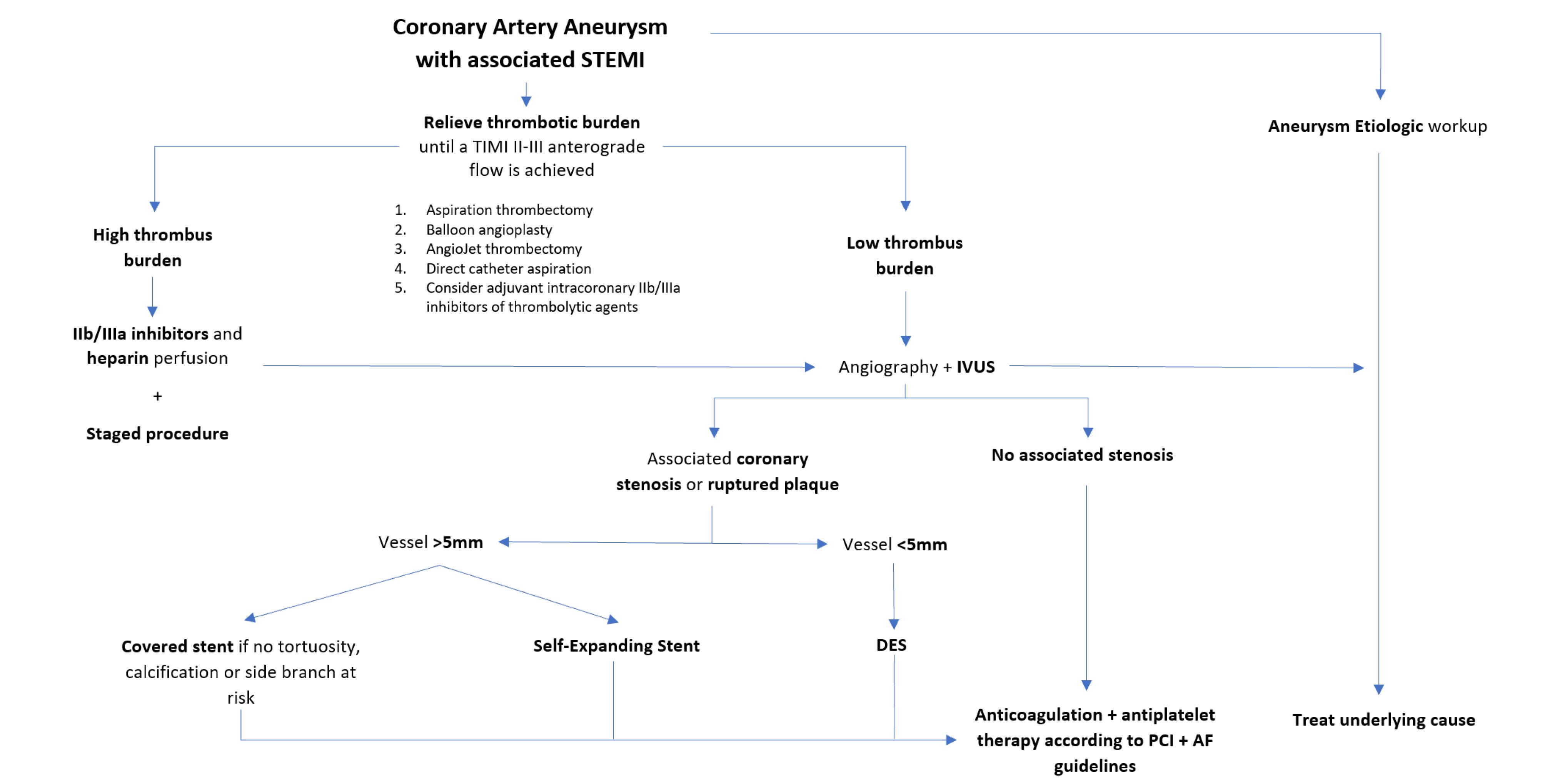
Figure 3.
Management algorythm of CAA associated with STEMI
.
Management algorythm of CAA associated with STEMI
Conclusion
In conclusion, thrombosed RCA aneurysms represent a challenging clinical entity, often presenting with acute coronary syndromes and requiring prompt diagnosis and intervention. Advanced imaging techniques, including echocardiography, cardiac CT, CAG, and MRI, play a critical role in the initial diagnosis, characterization, and management of these aneurysms. A tailored approach to treatment, guided by imaging findings and clinical context, is essential for optimizing outcomes in these patients.
Competing Interests
The authors declare no potential conflict o9f interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval
Written informed consent was obtained from the participant for anonymized patient information to be published in this article.
Supplementary Files
Supplementary file 1, Video 1 (PCI before thrombus aspiration)
(mp4)
Supplementary file 2, Video 2 (Thrombus aspiration POBA on distal
RCA)
(mp4)
Supplementary file 3, Video 3 (Follow-up CAG, 1 week post-PCI,
significant resolution of thrombus)
(mp4)
References
- Abou Sherif S, Ozden Tok O, Taşköylü Ö, Goktekin O, Kilic ID. Coronary artery aneurysms: a review of the epidemiology, pathophysiology, diagnosis, and treatment. Front Cardiovasc Med 2017; 4:24. doi: 10.3389/fcvm.2017.00024 [Crossref] [ Google Scholar]
- Matta AG, Yaacoub N, Nader V, Moussallem N, Carrie D, Roncalli J. Coronary artery aneurysm: a review. World J Cardiol 2021; 13(9):446-55. doi: 10.4330/wjc.v13.i9.446 [Crossref] [ Google Scholar]
- Crawley PD, Mahlow WJ, Huntsinger DR, Afiniwala S, Wortham DC. Giant coronary artery aneurysms: review and update. Tex Heart Inst J 2014; 41(6):603-8. doi: 10.14503/thij-13-3896 [Crossref] [ Google Scholar]
- Peng Y, Li Y, Jiang Y. Rare case of a giant thrombosed left anterior descending coronary artery aneurysm. J Cardiothorac Surg 2020; 15(1):204. doi: 10.1186/s13019-020-01250-8 [Crossref] [ Google Scholar]
- Eshtehardi P, Cook S, Moarof I, Triller HJ, Windecker S. Giant coronary artery aneurysm: imaging findings before and after treatment with a polytetrafluoroethylene-covered stent. Circ Cardiovasc Interv 2008; 1(1):85-6. doi: 10.1161/circinterventions.107.763656 [Crossref] [ Google Scholar]
- Vadalà G, Di Caccamo L, Alaimo C, Di Fazio L, Ferraiuoli G, Buccheri G. Coronary arteries aneurysms: a case-based literature review. Diagnostics (Basel) 2022; 12(10):2534. doi: 10.3390/diagnostics12102534 [Crossref] [ Google Scholar]
-
Madssen E. Coronary artery aneurysms. Tidsskr Nor Laegeforen 2023;143(15). doi: 10.4045/tidsskr.23.0315.
- Everett JE, Burkhart HM. Coronary artery aneurysm: case report. J Cardiothorac Surg 2008; 3:1. doi: 10.1186/1749-8090-3-1 [Crossref] [ Google Scholar]
- Kawsara A, Núñez Gil IJ, Alqahtani F, Moreland J, Rihal CS, Alkhouli M. Management of coronary artery aneurysms. JACC Cardiovasc Interv 2018; 11(13):1211-23. doi: 10.1016/j.jcin.2018.02.041 [Crossref] [ Google Scholar]
- Wang S, Song W, Wang B. A heavy ball: the rare giant right coronary artery aneurysm with thrombosis. Eur Heart J 2024; 45(40):4352. doi: 10.1093/eurheartj/ehae484 [Crossref] [ Google Scholar]
- Ishida S, Maeno G, Kato A, Wada Y, Okawa H, Sakurai T. Giant coronary artery aneurysm occluded completely by a thrombus. J Surg Case Rep 2024; 2024(5):rjae355. doi: 10.1093/jscr/rjae355 [Crossref] [ Google Scholar]
- van Steenbergen GJ, Klein F, Mast TP, Vlaar PJ, Teeuwen K. Large saccular aneurysm of the right coronary artery. Neth Heart J 2024; 32(5):221-2. doi: 10.1007/s12471-023-01847-3 [Crossref] [ Google Scholar]
- Khan Z. A young patient with acute ostial right coronary artery aneurysm presenting as ST elevation myocardial infarction. Cureus 2024; 16(4):e58063. doi: 10.7759/cureus.58063 [Crossref] [ Google Scholar]
- Jalalzai I, Kilic Y, Sönmez E, Çelik F, Erkut B. Giant right coronary artery aneurysm in a patient with multiple coronary artery aneurysmatic dilatations. Cureus 2023; 15(12):e51390. doi: 10.7759/cureus.51390 [Crossref] [ Google Scholar]
- Hennawi HA, Mathbout MF, Bidwell K, Nielsen CD. The curious case of an isolated right coronary artery aneurysm complicated by thrombosis and distal embolization. Glob Cardiol Sci Pract 2022; 2022(1-2):e202209. doi: 10.21542/gcsp.2022.9 [Crossref] [ Google Scholar]
- Teng P, Ni C, Sun Q, Ni Y. Giant right coronary artery aneurysm mimicking a right intra-ventricular mass: a case report. J Cardiothorac Surg 2020; 15(1):17. doi: 10.1186/s13019-020-1054-0 [Crossref] [ Google Scholar]
- Tham YC, Yap KH, Ch’ng JK. Large thrombosed right coronary artery aneurysm mimicking right atrial mass. J Cardiovasc Imaging 2019; 27(1):66-7. doi: 10.4250/jcvi.2019.27.e6 [Crossref] [ Google Scholar]
-
Arcinas LA, Yan W, Jassal DS, Love MP, Yamashita MH, Elbarouni B. Multimodality imaging of a giant right coronary artery aneurysm. Can J Cardiol 2018;34(12):1688.e5-1688.e7. doi: 10.1016/j.cjca.2018.08.031.
- Iannopollo G, Ferlini M, Koziński M, Ormezzano MF, Crimi G, Lanfranchi L. Patient outcomes with STEMI caused by aneurysmal coronary artery disease and treated with primary PCI. J Am Coll Cardiol 2017; 69(24):3006-7. doi: 10.1016/j.jacc.2017.04.030 [Crossref] [ Google Scholar]